Explore Counseling Today Articles
Crisis counseling: A blend of safety and compassion
When crisis strikes, clients need a counselor who can listen and share their heartbreak without inserting themselves into the situation, says Amanda DiLorenzo-Garcia, an American Counseling Association member and mobile response coordinator for the Alachua County Crisis Center in Gainesville, Florida. She describes crisis counseling as a short-term intervention to an acute situation with a singular purpose: ensuring that the client is safe and feels seen and heard.
Clients need someone who is “willing to be there, be present and be uncomfortable,” she explains. “We can’t help to fix the situation; all we can do is help the client to withstand it, to survive it — and often that’s heartbreaking. It challenges our humanity. … We have to stretch ourselves to be able to hold space for the immense emotions of despair, grief, hopelessness and helplessness, and that can be really uncomfortable to do.”
Part of life
Crisis counseling is a specialty within the counseling profession, but it’s also a skill that all counselors need to master because crises will pop up in everyday life for clients in all settings.
Thelma Duffey and Shane Haberstroh, in the ACA-published book Introduction to Crisis and Trauma Counseling, explain that crisis “is often an immediate, unpredictable event that occurs in people’s lives — such as receiving a threatening medical diagnosis, experiencing a miscarriage or undergoing a divorce — that can overwhelm the ways that they naturally cope.”
Crisis can also occur when multiple stressors are present simultaneously in a client’s life and a seemingly small incident, such as losing their keys and getting locked out of the house, pushes them to “the end of their rope” and sends them into a tailspin, says Ruth Ouzts Moore, an associate professor in the Counselor Education Department at the Chicago School of Professional Psychology.
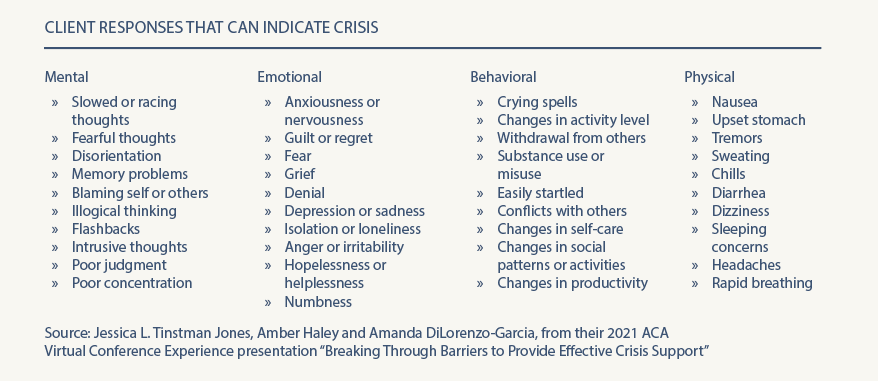
Shock, denial and disbelief are often the first emotions that clients experience in crisis situations, along with hopelessness and helplessness, says DiLorenzo-Garcia, who co-presented on “Breaking Through Barriers to Provide Effective Crisis Support” at ACA’s Virtual Conference Experience this past spring with Jessica L. Tinstman Jones and Amber Haley. A vast range of physical, mental, emotional and behavioral symptoms can indicate that a client is in crisis, she notes. (See list below.)
Moore defines crisis as the presence of a “risk of foreseeable harm” in a client’s life, either immediately or in the short term. The client may not automatically disclose this risk factor in counseling, however. Instead, their presenting concern can often be a “Band-Aid” or something more benign, she says, and it’s up to the counselor to “peel away the layers” to assess for risk. This can especially be the case with children, who may be referred to counseling for behavioral issues or because they’re falling behind at school. Sometimes, a crisis — such as abuse at home — may be the root cause of these struggles, notes Moore, an ACA member who specializes in working with children and adolescents who have experienced crisis and trauma.
Ali Martinez is a licensed marriage and family therapist and director of the Alachua County Crisis Center (where DiLorenzo-Garcia also works). In addition to mobile crisis response and in-person counseling services, the center operates a local 24/7 crisis hotline and responds to calls from their area of Florida to the National Suicide Prevention Lifeline. Most of the more than 45,000 calls the agency answers each year are from people who are feeling utterly alone as they face something that feels threatening to them, Martinez says. This includes losses that involve the death of a loved one as well as relational, financial and other losses.
“Most [callers] are not suicidal but are in some level of pain — experiencing something big that hasn’t been fully expressed, and they’re seeking space to do that,” Martinez explains. “They either are truly alone in what they are facing or feel alone in what they’re facing. They’re desperate for some sense of connection. They often know we can’t fix what’s happening — and that’s not usually what they’re seeking. …The struggle with crisis, what creates the danger and the true pain around a crisis, is the sense of how it disconnects us from people. The chaos, lack of control and strong emotions can make us feel alone. On the hotline, so often it’s trying to manage that chaos and find validation and connection — that what they’re feeling is a normal response to an abnormal situation. People often need someone outside their own world to let them know that what they’re feeling is OK and give them permission to express it.”
Crisis is self-defined
People can express their feeling of being in crisis very differently, but one common way that it manifests is tunnel vision, according to Martinez. In counseling, practitioners may hear a client who is experiencing a crisis speak with a narrowed scope or train of thought, returning to a singular experience or feeling over and over again.
Clients in crisis may feel like they’re drowning in emotions and that the issue that sent them into crisis is all-encompassing. Counselors may get the sense that their words are not getting through to the client because the client’s anger or despair is “filling the room,” Martinez says. Attending to the pain a client experiences during a crisis forces counselors to slow down their approach.
If counselors are “trying to get [the client] to look at the long term or take a bigger perspective and they can’t seem to do that and they keep coming back to that one painful thing, then we must change our approach and realize that this is the most important thing for them right now — and we have to listen for that,” Martinez says.
Above all, counselors must remember that “a crisis is defined by the person in it,” Martinez stresses. “For them, if it’s a crisis, it’s a crisis, and we have to honor that. Be aware that in that moment, we might have a much broader perspective on the possibilities [in the client’s life] and we might have good ideas about what could happen, but they may not be ready to hear it.” One of the most powerful things a counselor can say to a client in crisis is “tell me what this means to you,” she adds.
Martinez gives an example of a 12-year-old adolescent who is devastated after their first romantic relationship ends in heartbreak. As an adult, it would be easy for a counselor to tell the preteen client that this is the first of many heartbreaks life will bring. However, the client won’t be ready to focus on larger lessons about relationships and self until the counselor has helped them attend to their initial pain and despair over the breakup.
“For them, this is everything — feeling rejection and shame, sadness and despair. It doesn’t make it any less of a crisis experience for them,” Martinez says. “We [counselors] have to go in understanding it from their thinking.”
Josh Larson, a licensed professional counselor (LPC) in private practice in Denver, agrees that crisis must be self-defined by the client. He previously worked as a crisis clinician and operations and quality assurance specialist at Rocky Mountain Crisis Partners, a nonprofit organization that answers calls around the clock for several crisis hotlines, including the National Suicide Prevention Lifeline.
“We would always assure the caller that what they feel is a crisis, is a crisis. For one person, it could be that their cat got outside and they haven’t seen [the cat] for two hours and they’re feeling suicidal. For someone else, it’s something much bigger or more layered,” says Larson, an ACA member. “As a practitioner, even if what the client is telling us wouldn’t be a crisis for us, if they identify it as a crisis, then we need to treat it as such.”
Freedom to speak authentically
There is no shortage of crisis counseling models and assessment tools in the professional literature for practitioners to draw from in their work with clients. The counselors interviewed for this article did not recommend any one particular model or framework over another. They instead encouraged practitioners to research and select the counseling approach that works best for their style and client population.
No matter the model — or even if no model is used at all — a competent crisis counselor should shape a session into an arc that begins with rapport building and ends with connecting the person with resources. This last step ensures that the client has a safety plan (if needed) and is aware of options for follow-up care, such as local counseling services, walk-in crisis clinics and emergency hotline numbers. In the middle of this arc, at the core and heart of the therapeutic interaction, counselors create a nonjudgmental and empathetic space for the client to talk about their situation and share their burden.
The client does most of the talking in crisis counseling sessions, with the majority of the time spent simply “letting them tell their story,” DiLorenzo-Garcia explains.
Given that some clients may experience suicidal ideation during a crisis, an important part of this work is becoming well-versed in suicide assessment. DiLorenzo-Garcia and the other counselors interviewed for this article recommend that practitioners weave questions about a client’s safety, including those focused on suicide assessment benchmarks and protective factors, throughout the conversation.
In some situations, crisis counseling can offer clients the much-needed freedom to make strong statements without feeling judged or censored, Moore notes. This includes the freedom to talk about feelings such as anger or thoughts of harming oneself that can have shame or stigma attached to them.
This was the case for a 15-year-old client Moore once counseled who had turned to drinking, taking drugs and other risky behaviors to deal with turmoil at home, including feeling powerless when his father was abusive toward his mother. In session, the teen, referring back to an invective his father had directed at him, asserted, “I want to be an asshole.” Moore didn’t flinch at the client’s use of profanity. Instead, she responded, “You’re not an asshole.” When she repeated her statement, the teen began to cry, releasing emotions that had been pent-up.
“He had a deep, deep level of anger, resentment and betrayal that we needed to talk through. He found freedom in being able to say those things in a safe environment,” Moore recalls. “It was freeing that he could speak so strongly and hear his counselor repeat it back.”
Many of the crisis calls DiLorenzo-Garcia’s team responds to are in the public schools. Sometimes they respond because a student has called the county hotline themselves, but most often it’s because a school staff member (a school counselor, principal, school resource officer or administrator) has called to request their help.
In such cases, DiLorenzo-Garcia often begins a one-on-one session with a student by explaining the context of why the school asked her to come and speak with them. She assures the student that they are not in trouble and that she’s there because people are concerned about them. For example, she may say, “This is what I’ve heard from your school counselor, but I’m curious what your perspective is. What’s going on for you?”
“That’s the door opener. I reassure them, ‘I don’t want to make any assumptions about you. Your experience is your own, and I want to understand,’” says DiLorenzo-Garcia, a postdoctoral scholar at the University of Central Florida whose dissertation was on the loss and growth experience of mass shooting survivors and their families.
If the client’s experience includes thoughts of suicide, allowing them to talk through how they truly feel can help both the client and counselor realize how serious those thoughts are, DiLorenzo-Garcia adds. Sometimes a client has thoughts of suicide but doesn’t want to die, which can be accompanied by feelings of shame or isolation. If a client has a concrete plan to end their life, talking that through can help determine whether or how soon the client might act on that plan — and the necessity for follow-up care.
Assessing client needs
Larson notes that a majority of the callers during his time at Rocky Mountain Crisis Partners were not suicidal. However, some callers would say at the start of the call that they were not suicidal, but as the conversation went on and they began to unpack the depth of their emotions, it would become clear they were in fact experiencing suicidal ideation, he says.
This aspect of crisis counseling is why it’s imperative for counselors to be familiar with and proficient in suicide assessment. A counselor should be able to assess for preparatory behaviors, substance use problems, a client’s internal and external coping mechanisms, and other benchmarks to determine next steps, including safety planning or follow-up counseling, DiLorenzo-Garcia says.
Moore says it is important to be knowledgeable about assessing for not only suicidal ideation but also homicidal ideation when clients are in crisis. She acknowledges that asking questions about homicidal intent can be uncomfortable for practitioners. However, counselors must keep in mind that when in crisis, clients could have thoughts about harming others as well as themselves, she says.
“Be comfortable asking those difficult questions: ‘Are you having thoughts of killing yourself or harming anyone else?’ Don’t sugarcoat it,” says Moore, who presented the session “One Size Doesn’t Fit All: Creative Strategies for Counseling Diverse Families in Crisis” at ACA’s Virtual Conference Experience.
Larson points out that, along with active listening, validation of a client’s concerns and assurance of safety, de-escalation is a large part of crisis counseling. This can include mini versions of deep breathing and other grounding skills that clinicians might use in long-term counseling sessions with clients.
It can be helpful to match the person’s affect level, Larson says. For example, a counselor shouldn’t respond to a person who is hysterical with a flat, monotone voice. Instead, mirror them with a tone that is slightly calmer to gradually de-escalate the situation, he advises. Similarly, a crisis counselor shouldn’t respond to a client who is monotone or expressionless with a bright, bubbly demeanor. Instead, mirror their tone at a slightly more expressive level to gradually lift their affect, he says.
In crisis counseling, de-escalation and being presented with the opportunity to talk through what they are feeling will be enough for some clients, Larson continues. Others will be looking for help with problem-solving, such as conflict resolution or next steps to take after receiving a crushing health diagnosis. But Larson finds that clients in crisis are usually looking for one or the other, not both. Therefore, he advises counselors to be upfront and ask those in crisis, “What do you need? Do you want someone to listen or [someone to] help you problem-solve?”
“If you offer solutions to someone who is not wanting them, it can escalate them further into crisis,” Larson adds. Instead, he may tell clients, “I’m listening, and I’m willing to offer solutions if that’s what you’re looking for.”
In cases of suicidal ideation, DiLorenzo-Garcia finds it helpful to focus on the short term with clients. For example, she may say, “It’s a lot to ask you to live forever or live until next year, but right now, let’s talk about if you can live to tomorrow. What might that look like? Can you withstand the pain you’re going through just for tonight? What would it look like to survive and come back to school tomorrow?”
The counselors interviewed for this article emphasize that it is critical to arrange for follow-up support after crisis sessions but say that involving law enforcement to conduct welfare checks on a person in crisis should be done only as a last resort.
“Always follow up with a person who is in crisis, even if your session ends well and it sounds like things are going to work out,” DiLorenzo-Garcia stresses. Her agency contacts each client within three days after the initial crisis counseling session to make sure they are supported and doing well. In school settings, she also debriefs the adults involved in the student’s care (e.g., parents, school counselor) to ensure they are aware of the student’s needs and any next steps after a crisis counseling session.
Client safety
Meredith McNiel, an LPC who co-wrote the chapter “Crisis and Trauma Counseling With Couples and Families” in Introduction to Crisis and Trauma Counseling, notes that during crisis counseling, practitioners should focus on client safety through three lenses:
- Feeling safe to express themselves fully in the crisis counseling session
- Feeling safe at home and in the world outside of the counseling session
- Feeling safe within their life, including protective factors and social connections
An important part of this focus, she says, is reminding clients (multiple times if needed) that the counseling session is a safe and confidential space to speak freely about what they are experiencing.
Clients may disclose dark and powerful thoughts, such as suicidal or homicidal ideation, during crisis counseling, and McNiel acknowledges that many counselors’ first instinct may be to refer these clients for more intensive care. However, practitioners need to push through this initial reaction to keep from breaking clients’ trust.
“If a counselor is worried or nervous or scared about handling a situation, the client will feel that,” McNiel says. “We need to be comfortable asking hard questions while keeping the client comfortable.” The counselor should allow the client to say what they need to in session and “hold that space” without trying to fix their situation, she stresses.
“In a suicide crisis session, many professionals might [automatically] think, ‘Where can we send you?’ and in my experience, that is an absolute last resort. If a client hears that they’re going to be hospitalized or referred out to someone they don’t know or trust, they can instantly lose trust with a counselor,” says McNiel, an ACA member with a private counseling practice in Austin, Texas. Instead, “allow the session to happen fully in the way the client needs to share or release and process, and go from there,” she advises. “I assure [the client] that if anything further needs to happen, we will decide that together. I will not take control of what’s going to happen. I remind them that they are in control of their circumstances.” (See more about the ethical guidelines regarding protecting clients from “serious and foreseeable harm” in Standard B.2.a. of the 2014 ACA Code of Ethics at counseling.org/ethics.)
Crisis counseling is “less clinical and more relational” than long-term counseling, explains McNiel, who was a crisis counselor at the University of Texas at San Antonio Academy for Crisis and Trauma Counseling during her LPC internship. Practitioners need to let clients share and talk through their experience “until it feels complete” — whatever that looks like for them.
To ensure that a client’s safety and comfort are the primary focus in crisis counseling, practitioners must be so familiar with assessment tools that they don’t need to read the questions off a piece of paper or computer screen, says McNiel, whose doctoral research was on college counseling work with students who were suicidal. “[Instead of] saying, ‘Hold on, I’m going to grab this checklist and ask you some questions’ … ask questions in a relational way and fill out the assessment afterward rather than stopping the flow of a session,” she says. Counselors should be “getting answers [from the client] through conversation rather than interrogation.”
For example, an assessment tool might prompt a counselor to ask the client, “Are you thinking about killing yourself?” Practitioners still need to ask direct questions about suicidal ideation, but couching those questions in a more conversational way aids in maintaining trust, McNiel notes. Alternatively, the counselor could say, “I can see and hear that you are really struggling with this situation. You’ve shared with me that you have thoughts about killing yourself, and that makes sense considering what you’ve been through. I’m wondering how close you are to doing that? How close are you to going home and following through [on those feelings]?”
“The difference [in phrasing it this way] is the compassion in the language surrounding those really heavy questions,” she notes.
At the conclusion of a crisis session, counselors should talk through next steps with the client, including addressing what the client would do if things became worse and a crisis resurfaced after the session, McNiel says. If the individual is a long-term client, she advises scheduling their next session and letting them know how and when to reach the counselor during nonbusiness hours, as well as providing crisis hotline numbers.
Martinez agrees that in crisis counseling, practitioners should resist the urge to “fix” the situation the client is facing. In addition, counselors should avoid viewing it as a linear cause and effect. This includes thinking of suicidal ideation in binary terms of yes or no.
“We have to think of suicide in a much broader continuum, a range of pain and despair,” Martinez says. “[Society’s] fear and the stigma around suicidality makes us think about it as an on-or-off switch, but it’s more complicated than that.”
By definition, crisis is chaotic and messy, and the goal of a crisis counseling session is to de-escalate and share that burden, rather than organize or reorder it. Martinez illustrates this with a metaphor of a jumbled pile of sticks on the ground. A counselor’s instinct might be to gather the sticks and assemble a neat structure for the client, she says. Instead, crisis counseling involves allowing the client to pick up the sticks, one by one, and assemble them however they need to — even if it’s just into another pile on the ground that, to an outsider, looks equally as messy. “That’s much more powerful than us trying to figure out where the sticks belong,” Martinez says.
If a counselor approaches a crisis counseling session with the goal of tracking a client’s story in context, the counselor will miss the client’s full range of emotions — and the chance to connect and help the client bear that pain, Martinez says. “We can get caught up in [feeling that] ‘I need to make sense of the story.’ But that’s our need, our desire. The client may not need that or be ready for that. … When they talk and are listened to, they often begin to make sense of it themselves.”
Take Care of Yourself
The counselors interviewed for this article agree that it is imperative for practitioners who engage in crisis counseling to take steps to avoid burnout. In addition to regular self-care, this can include ongoing supervision or consultation with colleagues as well as other methods to combat feelings of isolation and empathy fatigue that can easily overwhelm practitioners whose clients share such heavy and troubling topics.
Moore suggests counselors take steps to maintain a balanced caseload and stay aware of how stress and burnout manifest for them personally. “Doing trauma and crisis work is heavy stuff. It can be super rewarding but super draining,” Moore says. “We carry [clients’] trauma with us, so it’s important to take care of ourselves. … Sadly, we need more and more counselors to do crisis work, and if you don’t take care of yourself, that’s one less counselor to help people who need it.”
It’s also important to remember that sharing the burden of crisis with clients is a gift, Larson says. A crisis counselor may be the only person the client feels they can talk to during their lowest moments.
“It takes a lot of courage to pick up a phone and tell a stranger [a crisis counselor] that you want to die,” Larson says. “Always remember that it’s an honor and privilege to hear people’s hardest stuff — their deepest, darkest secrets.”
 ****
Contact the counselors interviewed in this article:
****
Contact the counselors interviewed in this article:
- Amanda DiLorenzo-Garcia: amanda.dilorenzo@ucf.edu
- Josh Larson: josh@emotional-nutrition.com
- Ali Martinez: amartinez@alachuacounty.us
- Meredith McNiel: dr.meredith@essencetherapyatx.com
- Ruth Ouzts Moore: rouztsmoore@thechicagoschool.edu
- Assessment, Diagnosis & Treatment
- Trauma & Stress-Related Disorders
- Counselors
Search CT Articles
Filter CT Articles
Current Issue
Sign Up for Updates
Keep up to date on the latest in counseling practice. Sign up to receive email updates from Counseling Today.